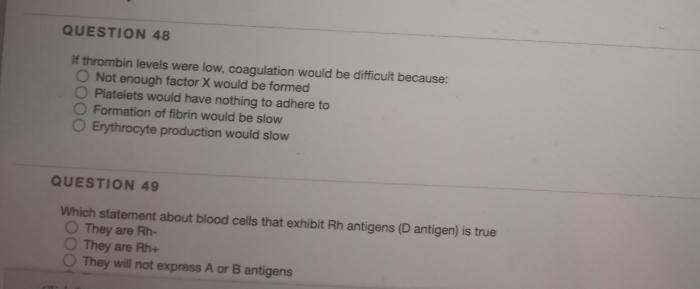
If thrombin levels were low coagulation would be difficult because – If thrombin levels were low, coagulation would be difficult because thrombin is a crucial enzyme in the coagulation cascade. It converts fibrinogen to fibrin, which forms the meshwork that traps platelets and creates a stable blood clot.
Without adequate thrombin, fibrin formation is impaired, leading to difficulties in coagulation. This can result in excessive bleeding and an increased risk of hemorrhagic complications.
Thrombin’s Role in Coagulation
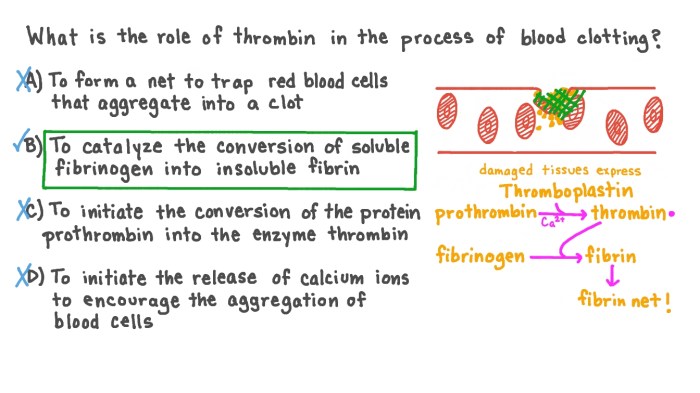
Thrombin, a crucial serine protease enzyme, plays a pivotal role in the coagulation cascade, the intricate process responsible for blood clot formation. It catalyzes the conversion of soluble fibrinogen into insoluble fibrin, the primary component of blood clots. This transformation initiates the formation of a stable fibrin mesh, trapping platelets and red blood cells to form a hemostatic plug.
Thrombin’s Mechanism of Action
Thrombin exerts its function by cleaving two specific sites on the fibrinogen molecule, designated as fibrinopeptides A and B. This cleavage exposes polymerization sites on the fibrinogen molecule, enabling them to interact and form long, insoluble fibrin strands. These strands entangle and cross-link to create a dense network, providing the structural integrity of the blood clot.
Consequences of Low Thrombin Levels
Impaired thrombin production or activity can significantly hinder fibrin formation, leading to difficulties in coagulation. This condition is known as hypofibrinogenemia, which can manifest as excessive bleeding or impaired clot formation.
Impact on Fibrin Formation, If thrombin levels were low coagulation would be difficult because
Low thrombin levels directly impact the conversion of fibrinogen to fibrin. Reduced thrombin activity leads to insufficient fibrin production, resulting in a weakened and unstable clot. This can manifest as prolonged bleeding time, increased blood loss, and impaired wound healing.
Clinical Implications
Hypofibrinogenemia can be caused by inherited disorders, such as afibrinogenemia and dysfibrinogenemia, or acquired conditions, including disseminated intravascular coagulation (DIC) and liver disease. Inherited disorders result in a deficiency or dysfunction of fibrinogen, while acquired conditions can lead to its consumption or degradation.
Factors Influencing Thrombin Production: If Thrombin Levels Were Low Coagulation Would Be Difficult Because
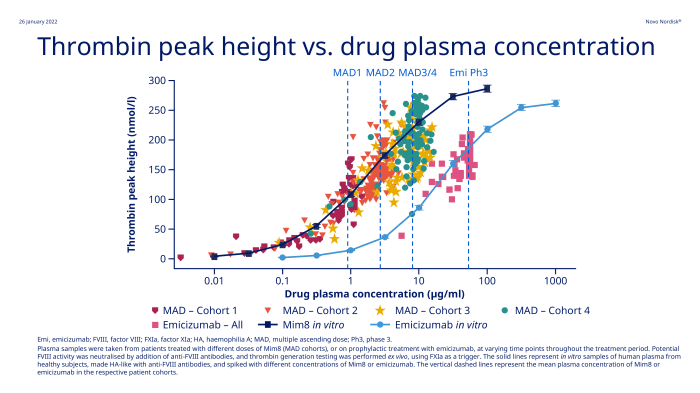
Thrombin production is regulated by a complex interplay of factors, including:
- Thrombin activators:These factors, such as factor Xa and factor Va, convert prothrombin to thrombin.
- Thrombin inhibitors:These factors, such as antithrombin and protein C, regulate thrombin activity and prevent excessive clot formation.
- Cofactors:Factors such as calcium ions and phospholipids are essential for thrombin activity.
Deficiencies and Abnormalities
Deficiencies or abnormalities in these factors can lead to low thrombin levels. For instance, a deficiency in factor VIII or factor IX, which are involved in the activation of factor X, can impair thrombin production. Similarly, a deficiency in antithrombin can lead to excessive thrombin activity and consumption, resulting in hypofibrinogenemia.
Therapeutic Implications
Therapeutic strategies for low thrombin levels aim to restore hemostasis and prevent excessive bleeding. These strategies include:
- Thrombin replacement therapy:This involves administering purified thrombin or recombinant factor VIIa, which directly converts prothrombin to thrombin.
- Drugs that stimulate thrombin production:These drugs, such as tranexamic acid, inhibit fibrinolysis, thereby preserving existing clots and promoting clot formation.
Specific Medications
Specific medications used for thrombin replacement therapy include:
- Recombinant thrombin (Thrombin-JR)
- Recombinant factor VIIa (NovoSeven)
Tranexamic acid is a commonly used antifibrinolytic agent.
Case Study Analysis
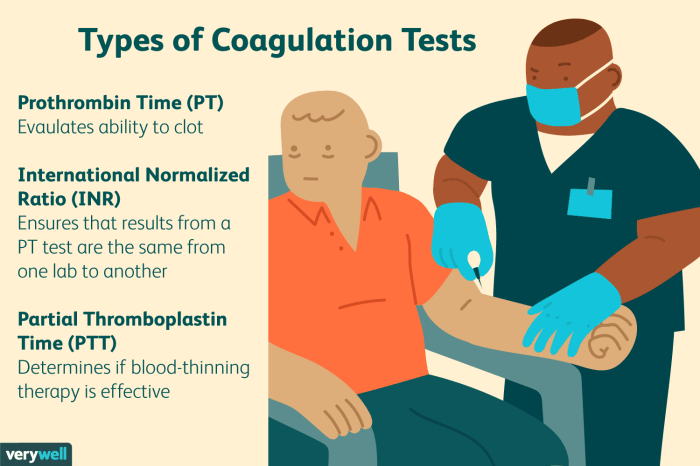
Case Presentation:A 65-year-old male presents with a history of excessive bleeding after a minor laceration. Laboratory tests reveal prolonged prothrombin time (PT) and activated partial thromboplastin time (aPTT), and a low fibrinogen level.
| Clinical Presentation | Laboratory Findings | Treatment Plan |
|---|---|---|
| Excessive bleeding | Prolonged PT and aPTT | Thrombin replacement therapy (Recombinant thrombin) |
| Low fibrinogen level | Tranexamic acid (antifibrinolytic agent) |
Challenges and Considerations:Managing patients with low thrombin levels requires careful monitoring of coagulation parameters and prompt intervention to prevent excessive bleeding. The choice of therapy depends on the underlying cause of hypofibrinogenemia and the severity of bleeding.
Common Queries
What are the consequences of low thrombin levels?
Low thrombin levels can lead to impaired fibrin formation, resulting in difficulties in coagulation and an increased risk of bleeding.
What factors can influence thrombin production?
Thrombin production is regulated by various factors, including the availability of fibrinogen, the activity of thrombin inhibitors, and the presence of cofactors such as calcium and phospholipids.
How is low thrombin levels treated?
Treatment for low thrombin levels typically involves thrombin replacement therapy or the use of drugs that stimulate thrombin production, such as prothrombin complex concentrates or factor XIII concentrates.